I might be squinting at the issue too hard, but my takeaway from this well-done USA Today piece about the legal battle over copay accumulators is that, maybe, the Biden administration is not going to throw its full support behind copay accumulators.
Quick background: in September, a federal judge ruled that insurance companies shouldn’t be able to refuse to count copay assistance toward deductibles or OOP maxes. This was a victory for patient advocates, who hate that insurance-plan tactic — copay accumulators — for obvious reasons. But then, last month, HHS made a couple of legal filings suggesting it would appeal the decision and refuse to implement the judge’s ruling.
The USA Today story had HHS walking back that position. Maybe. A little. Perhaps.
In comments to the newspaper, an HHS spokesperson said that the government hadn’t committed to appealing the ruling … the legal filing was just a matter of keeping options open. And the refusal to enforce the decision was more an acknowledgment that the government wasn’t going to take action while it drafts a new rule.
Now, that could be spin. That could be a realization that screwing patients over by defending a policy of the previous administration is bad politics. It could be that nothing is changing. But it certainly doesn’t sound like this is a fight that HHS is particularly pumped about.
I flagged the CVS move to cost-plus pricing (for pharmacies, not consumers) yesterday, and that ended up being the hot story yesterday, with pretty much everyone following up on the WSJ exclusive.
There are two ways to look at the story.
One way is on the merits: will this CVS action change the playing field when it comes to drug pricing and reimbursement? There was some solid reporting there. I liked this skeptical take from STAT that suggested that this may be as much about financial engineering as transparency. And this is the sort of thing where Adam Fein is always helpful in explaining the underlying supply chain dynamics.
That skepticism is beginning to break through. This two-minute clip from CNBC this morning is worth watching, not (just) because it gives air time to PhRMA’s statement but because the back-and-forth between the anchors suggests that people are starting to understand the ways that the system is broken.
The other way to think about this is from the POV of media criticism. I’m not going to name names here, but this is a story that received a lot of coverage where it felt like the reporters involved had a shaky understanding of how the system is built.
That’s not a complaint or an accusation! This stuff is legitimately hard (as you all know, I get it wrong plenty). Instead, I’m bringing this up because it suggests that, on super-complicated drug-pricing issues, it’s easy for the public to be spun (or confused). There’s no easy answer to fixing that, but the first step is to recognize the dynamic.
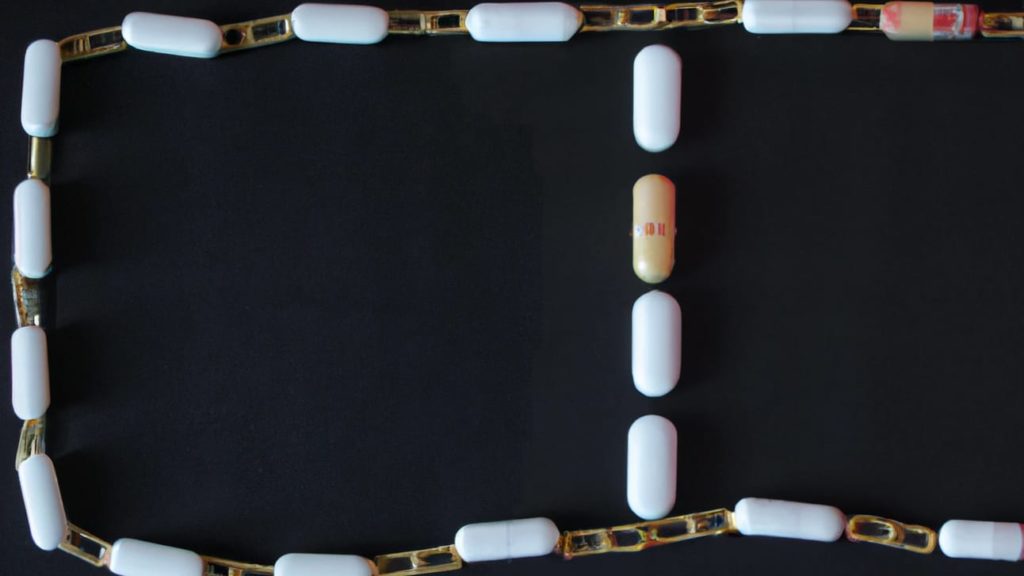
Man, I do not like seeing stories like this one, about formerly cheap medicines reintroduced at hugely increased prices.
There may be an argument to be made about value and the importance of ensuring supply, but a) no one bothered to make that argument (the company involved didn’t speak to the press) and b) I suspect the reputational damage to the entire system far exceeds whatever financial benefit might accrue. I don’t like linking to this kind of stuff, but these are the kinds of stories that drive perception of the industry and thus merit consideration.
Related thought experiment: Would the IRA have passed if not for Martin Shkreli’s antics way back in 2015?
“How big will the obesity drug market be” is a fun question that lends itself to absurd calculus and outrageous headlines, which makes this STAT story about analysts who are a bit more measure a useful corrective. To be clear: no one thinks this isn’t going to be a monster category, but there are a lot of unknowns between “monster” and “unfathomably gargantuan.”
Speaking of obesity, this is a fun STAT op-ed about a revolutionary way to pay for medicines that involves low upfront annual prices followed by a giant one-time payout late in a patient’s life. It’s too complex to summarize here, and it is beyond implausible for a thousand reasons. But I’m a huge fan of anyone willing to throw out-of-the-box ideas out there.
One more obesity thing: new research shows that adherence to GLP-1 medicines is a lot better than adherence to older weight-loss drugs. I’d written up older research that suggested that the number of people who just don’t fill their scripts was huge, but it may be that GLP-1s, for presumably obvious reasons, won’t follow that pattern.
Colorado’s PDAB will vote on Friday if Trikafta is “unaffordable.” The packet of information that will be used in the deliberation is online here.
Maureen Testoni from 340B Health has an op-ed out defending the 340B program by highlighting the way that 340B has kept drug-price inflation in check. But these kinds of op-eds are always fascinating in what they don’t say. In this case, there is absolutely no rebuttal to the arguments that the 340B program has become overbroad and fails to benefit patients.
I don’t know what Sen. Bill Cassidy is driving at by this open call for thoughts on gene therapy coverage and access, but here is Cassidy’s list of almost 60 questions that he’s looking for answers on.
Good wonkery here from NPC’s John O’Brien and Genentech’s Jan Hansen on some of the unanswered questions on how CMS will deal with “therapeutic alternatives” in the IRA price-setting process.
I respect the hell out of Mark Cuban’s hustle, but he’s not the 13th most influential person in health care. But I’m also not sure that my perspective on things is aligned with Modern Healthcare.
If this email was forwarded to you, and you’d like to become a reader, click here to see back issues of Cost Curve and subscribe to the newsletter.