The Colorado Prescription Drug Affordability Board blinked. On Friday, they had a chance to deem Vertex’s CF drug, Trikafta, as the first-ever “unaffordable” medicine, thereby opening the medicine to price controls. But they didn’t, voting unanimously that Trikata was “not unaffordable.”
That’s a huge win for patients, and it didn’t come without a lot of effort from the advocacy community to make two clear points. The first was that Trikafta is a medical marvel and the exact kind of innovation that we should want to encourage. The second was that access for Trikafta is solid, and it’s probably unwise to mess with a system that is working for patients.
Both of those arguments seemed to hit with the board members, but it’s the second one that is most interesting to me.
The board’s deliberations seemed to turn, in part, on the fact that there was no real evidence that patients were being harmed by the current system. There were no stories of patients who needed the medicine but couldn’t get it for cost or other reasons.
In other words, the vote ultimately turned not on the squishy question of “affordability” but rather the more meaty question of “access.”
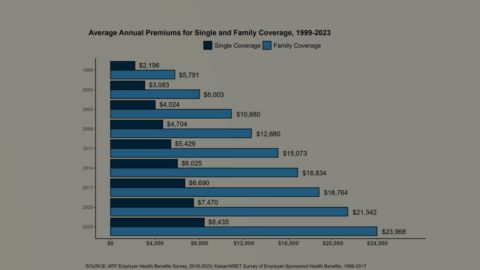
That’s a two-edged sword. Because though there don’t appear to be huge access issues with Trikafta in Colorado, that’s not the case for every medicine. But where there are access issues, it’s often not a question of drugmaker actions, but rather insurance coverage and design. If only states were spending as much time on fair access as they were on “affordability.”
ICER is out with their latest report purporting to show medicines with “unsupported price increases.” I’ve been complaining about this effort for so long that it’s hard to write anything that doesn’t feel repetitive.
But the SparkNotes version is that the UPI report uses a lousy methodology to address the increasingly inconsequential issue of drug price increases. Between the IRA’s inflation penalties and the increasingly tough market environment, it really doesn’t feel like this is an effort that anyone needs.
In fairness, this is not, philosophically, a ridiculous effort. Understanding how the cost-benefit ratio of a given drug changes over time, given changes in price and knowledge base, is an incredibly interesting question. But that’s not what ICER is doing (or claims to be doing). Instead, it’s sloppy methodology built on crappy data.
My issue has always been that the report relies on net price data from SSR Health. That data is pretty good, but it’s just not good enough or reliable enough for the way that ICER uses it. In the past, ICER used to fess up about the places where the SSR data was unreliable, but ICER doesn’t do that any more (I went into this in a little more depth on this on LinkedIn today).
NPC doesn’t like it, either, and you can read their comments here. STAT also has coverage.
My hope — and this has been my hope for years — is that ICER will walk away from this effort in the future. They have better ways to spend their money.
Extra quick today:
We might get a PBM-reform vote in the House this week. Fierce details what’s at stake.
There is a lot to unpack in the value and pricing decisions around the two new sickle-cell disease gene therapies approved on Friday, Vertex’s $2.2 million CRISPR-based approach and bluebird’s $3.1 million treatment.
The Cigna-Humana thing is not happening, per WSJ. This is probably good news for the PBM industry, which won’t have to endure the months of FTC sniping around the merger. (There will still be plenty of FTC sniping. The FTC will just have one less thing to shoot at.)
Novo Nordisk filed for summary judgment in its IRA case. Nothing earth-shattering in the brief,
If this email was forwarded to you, and you’d like to become a reader, click here to see back issues of Cost Curve and subscribe to the newsletter.